Global Key Message
- All countries should ensure access to cancer drugs on the WHO Model List of Essential Medicines that are low-cost and effective. Access and affordability of essential cancer medicines can be facilitated through the adoption of policies that support the use of generic medicines.
- Access to new, patented, and expensive NCD medicines should be considered on an individual basis based on priorities identified within national cancer control planning with the number and variety of cancer medicines increasing with the level of available resources.
- Radiotherapy is a critical component of high-quality cancer care. It can cure cancers alone, or in combination with surgery or chemotherapy.
- All governments have approved the Global Monitoring Framework for Non-communicable Diseases (NCDs) that recommends adoption of the global target of an 80% availability of the affordable basic technologies and essential medicines, including generics, required to treat major NCDs in both public and private facilities.
- Progress will be measured by monitoring the availability and affordability of quality, safe and efficacious essential NCD medicines, including generics, and basic technologies in both public and private facilities.
The Facts
- Household surveys show that 41–56% of households in LMICs spend all of their health-related expenditure on medicines. The cost of cancer medicines does not have to be prohibitively expensive - most of the off-patent generic cancer medicines required for LMICs are available for less than $US100 per course of treatment, and nearly all for under $US10005.
- Radiotherapy is recommended in 52% of new cancer patients. In LMICs, the need for RT may in fact be higher due to a more advanced stage of disease at presentation. There is currently a deficiency of at least 5,000 radiotherapy machines in LMICs. This shortage means that up to 70% of cancer patients in LMICs who may benefit from radiation medicine do not receive this essential curative or pain relieving treatment.
- Access to essential cancer medicines and radiotherapy falls dramatically short of demand, most notably in low- and middle-income countries (LMICs) resulting in unnecessary suffering and deaths from cancers that are treatable in high-resource settings.
- Data reported from 36 LMICs showed that the mean availability of NCD generic medicines was 36% in the public sector and 55% in the private sector (but at a much higher price). High-income countries consume 93% of the world’s morphine supply while 65% of deaths from cancer occur in LMICs.
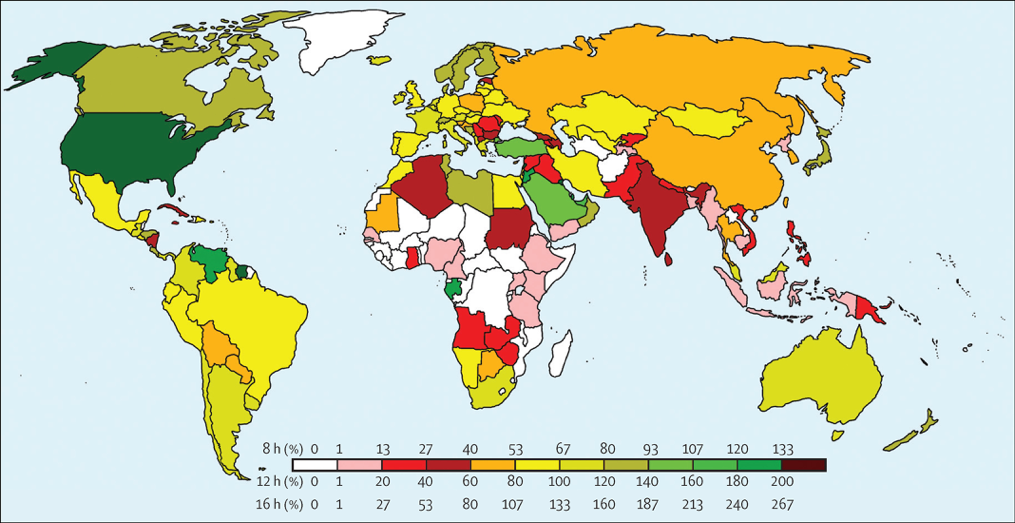
Coverage of radiotherapy services according to country as determined by global equipment databases, an activity-based operations model, cancer incidence, and evidence-based estimates of radiotherapy need. Estimates depend on the nature of equipment use. The colour bar shows the operational model: 12 h operation was used as the feasible case, but 8h and 16h were also modelled to capture typical and potential capacity, respectively.
Figure taken from “The Lancet Oncology: Expanding global access to radiotherapy, Vol 16, September 2015, p. 1168”
Meeting the Challenge
The safe and effective delivery of cancer medicines and radiotherapy, as part of a team-based approach to cancer care, is achievable in both high- and low-income settings if implemented as part of a national cancer control plan and according to evidence-based clinical guidelines that are appropriate for the level of resources.
Target population: Investments in the necessary infrastructure and a skilled and supported health workforce should be priorities. These should include the development of laboratory, pathology, and clinical services for cancer diagnosis, staging, and monitoring of effectiveness and safety of chemotherapy; additional radiotherapy equipment to address overall capacity constraints and to replace out-dated, less effective, machines; and education and training of healthcare professionals.
Data Availability: The WHO Model List of Essential Medicines for adults (EML) and children (EMLc) presents a set of medicines that are considered to be cost-effective and of critical public health importance in all countries. In informing national pharmaceutical policies, the WHO Model List serves as a key lever to improve access to essential medicines including cancer medicines worldwide. A review is considering a new structure for the section on cytotoxics and adjuvant medicines to ensure that the list best reflects the cancer medicines that are most essential for patients worldwide. Furthermore, radiotherapy is often perceived as a complex and expensive solution. However, a lack of investment in this critical treatment modality will exacerbate the burden of cancer and reinforce the disparities in access to cancer care.
Resources mobilisation: National cancer planning processes should identify a list of essential cancer medicines for training, supply, and reimbursement in conjunction with the development of evidence-based national clinical guidelines. Ensuring access to quality cancer medicines requires national authorities to also consider mechanisms to increase efficiency in procurement, supply, and use to promote access to medicines within the existing health budget. Greater awareness is needed amongst policy makers, health professionals, patients and caregivers of the increasing benefits of using modern radiotherapy. Radiotherapy has been shown to be a cost-effective approach to cancer treatment in high-income countries, and evidence to further support cost-effectiveness is also emerging from developing countries.
Key Tools
Global Task Force on Radiotherapy for Cancer Control (GTFRCC) (LINK)
WHO Model List of Essential Medicines 2019 (PDF)
WHO Model List of Essential Medicines 2017 (PDF)
WHO Model List of Essential Medicines 2015 (PDF)
Proposing Essential Medicines to Treat Cancer: Methodologies, Processes, and Outcomes
Country examples
Cancer is increasingly recognized as a major public health problem across Africa. The burden of the disease is worsening as rising living standards lead to lifestyle and environmental changes, such as unhealthy diets, physical inactivity and pollution, that increase the incidence of cancer.
For many years, Mauritania, one of Africa’s 34 least developed countries, has struggled to address the human and financial costs of cancer. Haematological malignancies and solid tumours, for example, require specialized treatments that were not available at Mauritanian hospitals, which meant that patients had to seek treatment abroad. Cancers of the cervix, breast, prostate, liver and ovary are among the most common cancers in the country. After establishing a National Oncology Centre (CNO) in Nouakchott in 2010, the Government of Mauritania sought IAEA support to build capacities in the delivery of radiotherapy, nuclear medicine, and cancer care, generally. The specialized medical staff—radiation oncologists, medical physicists, radiation therapy technologists—trained abroad by the IAEA, are now fully in-charge of the facility.
On November 28, 2014, the completed nuclear medicine facility was inaugurated. Like the radiotherapy centre, it is located within the National Oncology Centre in Nouakchott.
For more information regarding this IAEA project download the pdf.
