Global Key Messages
- Due to population ageing and trends in risk factors, the number of people diagnosed with cancer is growing. About 14 million new cases of cancer are diagnosed worldwide each year. At the global level, in 2012, 32.6 million people were five-year cancer survivors (people who are alive five years after being diagnosed with cancer), including 15.6 million in developing countries (Globocan).
- Survival for many cancers has improved over the last 20 to 30 years. Together these trends mean that an increasing number of people are living with or beyond cancer.
- Cancer survivors face a number of key challenges within health care systems in terms of receiving appropriate and adequate access to care. Evidence suggests a significant number of people with a lived experience of cancer have unmet informational, psychosocial, and physical needs which can be effectively addressed through supportive care interventions.
- In low income countries and some middle income countries where infrastructure and access are still an issue, rates of survivorship are still relatively low. (1)
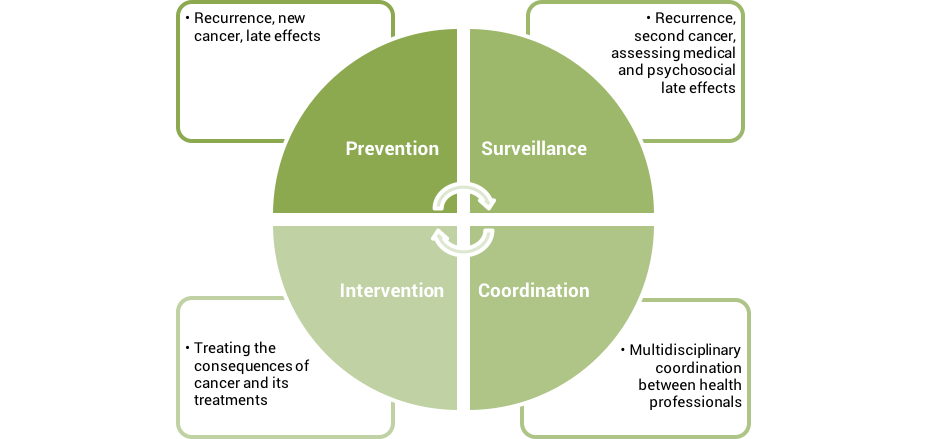
- Cancer survivors require long-term surveillance, risk assessment and primary prevention as well as risk reduction for secondary cancers (2), as many face distinct and serious health care issues related to the cancer itself, pre-existing comorbidities, and the exposure to therapy (radiation (3) and chemotherapy (4)). Delivering high quality survivorship and supportive care can enhance patients’ long term health by managing concerns related to cancer treatment and survivorship.
The Facts – Key data
- Survivorship and Supportive care can broadly be defined as services, which address a patient’s informational, emotional, spiritual, social, or physical needs during the diagnostic, treatment, or follow-up stages of cancer even after treatment, and throughout the rest of their life. Survivorship is inclusive of the idea of Patient-Centered Cancer Care, or care that is “respectful of and responsive to individual patient preferences, needs and values, and ensures that patient values guide all clinical decisions.” (Institute of Medicine, 2001; 2013)
-
Survivorship can be divided in three phases that describe the period a survivor is going through: acute survivorship, extended survivorship and permanent survivorship. “Acute survivorship begins at diagnosis and goes through to the end of initial cancer treatment. Cancer treatment is the focus. Extended survivorship begins at the end of initial cancer treatment and goes through the months after. The effects of cancer and treatment are the focus. Permanent survivorship is the period when years have passed since cancer treatment ended and recurrence seems less likely. Long term effects of cancer and treatment are the focus. (http://www.cancer.net/survivorship/about-survivorship)
Supportive care theories and practice concern issues of health promotion and prevention, survivorship, palliation, and bereavement, and can be categorised as primary, secondary, or tertiary care depending on the level of specialization.
Hewitt M. et al., From Cancer Patient to Cancer Survivor: Lost in Transition, NAP, 2005.
Meeting the Challenge
Elements of Patient-Centered Cancer Care
The Elements of PCCC are a collection of key building blocks that can be utilized to deliver cancer care across a variety of settings. Across the cancer continuum, the following elements characterize cancer care that is patient-centered; that is, care that is respectful of and responsive to the needs, preferences, and values of cancer patients, survivors, and their family members and caregivers:
1.Cancer care which incorporates best practices and new evidence as they are generated.
- Rapid, efficient, and continual incorporation of new evidence into clinical guidelines; patients have access to safe, efficient, equitable, high-quality care at all times.
2. Providers who identify and communicate realistic goals to the patient and their family and caregivers.
- Patients, family, and caregivers feel informed. Uncertainty is minimized, and when uncertainty exists, a timeline is estimated as to when answers will be available. Questions are answered, even when the answer is “We don’t know yet.”
3. The needs, preferences, and values of the patient – including sociocultural, socioeconomic, and spiritual – are continually assessed and serve as the foundation of care decisions.
- Patients are considered as “whole people,” treated with dignity and respect. Their needs, preferences, and values, both current and those that existed before their cancer diagnosis, are assessed and responded to as processes of care unfold.
4. A technology-enabled learning health-care system that uses data capturing patient reported outcomes (PROs) to support the provision of care, both during and between clinical encounters.
- PROs are securely and systematically captured at the point-of-care and in between clinical encounters, either in response to prompts from the health care team or as patient-initiated reports. Technology is used to optimize the process of capturing PROs and integrating the PRO data into workflows, communications (including patient-provider communication), and decision making, and to support connections between research and clinical care (e.g., clinical trials). Technology enhances – but does not replace – the patient’s relationship with their health care team.
5. Providers, patients, and individuals the patient grants permission to have timely and no-cost access to up-to-date medical information (including access to the patient’s medical record).
- Ideally, a secure, patient-facing portal gives patients (and, with their permission, their family members and caregivers) constant access to their medical data. When medical records are requested, they are provided within four business days of the information being available to the provider (or within 36 hours of discharge from the hospital) and there is no cost to the requestor.
6. Accessible, timely, clear, and effective communication between all parties engaged in the care of the patient and, with the patient’s permission, their family and caregivers.
- It is not the patient’s responsibility to coordinate information exchanges about their care from one provider to another. Members of the care team have clear and open lines of communication and proactively update each other about the status of the patient. Providers aim to communicate with patients and families in ways that are sensitive to the patients’ sociocultural and socioeconomic contexts, that engender trust, and that enact the core components of patient-centered communication in cancer care.
7. Survivorship Care Planning, including provision of treatment summaries, survivorship care plans, psychosocial care plans.
- Survivorship care planning is integrated into care and related care plan documents are provided to patients in their preferred format and with adequate explanation and support.
8. Education and support to empower the patient’s preferred level of participation in informed decision making.
- To the degree that they want to participate and want their family members and caregivers to participate, information and time are provided to support autonomy and decision making related to cancer care.
9. Coordinated, integrated care across multiple disciplines within and outside of oncology (including primary care and allied health professionals).
- Cancer care often involves multiple health professionals. The decisions made by one are understood and accommodated by the others. When necessary, communication to reach agreement, coordination, and integration takes place in a timely manner. Special attention is given to avoid problems developing during transitions in care.
10. Counseling and support for managing practical concerns related to cancer such as access to transportation; financial needs; insurance; child care, and advanced directives.
- Practical concerns are acknowledged as being as important as physical and emotional concerns. Proactive support is offered to help patients manage practical issues that result from cancer and receipt of care.
11. A positive therapeutic alliance between patients, their family, their caregivers, and the health care team.
- The culture of care appreciates that positive relationships and communication with the health care team are important for patients, their family, and their caregivers. The therapeutic alliance is grounded in trust and fostered through mutual agreement on the goals of treatment, including agreement on when the goals of treatment need to change over time.
12. Access to family planning services, such as fertility preservation, reproductive assistance, and adoption support.
- Patients and their families are proactively counseled about risks to fertility and sexual health as part of treatment planning and provided appropriate referrals to fertility preservation and counseling resources.
13. Access to genetic testing and counseling.
- Patients are aware of genetic testing and counseling services, the degree to which genetic testing and counseling are appropriate for/indicated in their care, and how to access them.
14. Emotional and psychosocial support for the patient and their family and caregivers.
- The emotional and psychosocial impact of cancer and its treatment are acknowledged and anticipated. Multiple levels of support, including peer counseling (face-to-face or technology-mediated), professional counseling, and psychiatric intervention are available and accessible.
15. Supportive care, including preventive care (e.g., care to support nutrition, physical activity) and to promote self-management.
- Promoting health, wellness, and self-management/self-care are critical even when someone is being treated for disease. Patients are provided with care to support health and wellness to foster optimized responses to treatment and best chances for healing and recovery when treatment ends.
16. Access to complementary and alternative medicine.
- Patients are aware of and can access a wide range of complimentary and alternative medical interventions, including but not limited to massage, acupuncture, body work, and art-based therapies.
17. Access to palliative care.
- Pain control and symptom management are central to care. Palliative care is offered early and often to support as comfortable an experience as possible during treatment.
18. Access to comparative information about the costs of care before care is provided.
- Affordability of cancer care includes managing costs associated with provision of care and the ancillary costs associated with participating in care (e.g., transportation; absence from work). Before care is delivered and as part of information used to make decisions about care, either by relevant staff in the health care system or in collaboration with a representative from the patient’s health insurance, patients are provided information about the cost of the care and given comparative cost information for comparable interventions.
19. Reasonable wait times before appointments begin and to secure future appointments.
- Patients wait less than 2 hours before a scheduled appointment begins and are able to get a new appointment scheduled within 2 weeks of their desired date.
20. Support to establish and/or maintain healthy sleep both at home and in the inpatient setting.
- Sleep is integral to health. Patients are given support – including behavioral and medical intervention – to promote healthful sleep at home. During inpatient stays, measures are taken to make the environment conducive to healthful sleep.
21. Architecture or a built environment that is designed to promote a patient-centered experience.
- Whenever possible, built environment design decisions are made to create settings that support a nurturing care experience for both patients and providers, with an emphasis on design features that support communication, comfort, connection to nature, privacy, and care coordination. Patients served by and staff working in the environment are consulted early and often for input.
22. Education, support, and training for all staff to support of the implementation and provision of patient-centered cancer care.
- For all staff that interacts with patients – medical and non-medical – regular opportunities for training to provide a patient-centered experience are offered and participation is incentivized. Prioritization for training opportunities is informed directly by feedback from patients, their families, and caregivers.
23. Continuous quality improvement and performance measurement, including the integration of new standards as they evolve.
- Achieving high-quality patient-centered cancer care is a moving target. To ensure continually hitting the mark, ongoing performance measurement is used to direct continuous quality improvement and the achievement of new standards of care, with measurement and outcomes tracked using electronic infrastructure and with guidance from patients and relevant policy and leadership groups such as the Affordable Care Act and the Quality Oncology Practice Initiative. Transparency related to the communication of these efforts to the patient population served and the broader community is valued.
Key Tools
Country Example
The following LIVESTRONG videos discuss delivering patient-centered cancer care, its challenges and successes in the US:
