Global Key Messages
- In countries with a high incidence of cervical and liver cancer, access to safe, effective and affordable vaccines for HBV and HPV should be introduced in national immunisation schedules and NCCPs.
- The World Health Organization (WHO) recommends that vaccination against HBV infection is included in national infant vaccination programmes, with 3 doses including 1 within 24 hours of birth is the most effective way to tackle chronic HBV infection.
- The WHO recommends HPV immunisation targeted at young adolescent girls aged 9 to 13 years in countries where cervical cancer constitutes a public health priority and where vaccine introduction is feasible, where sustainable financing can be secured and when cost-effectiveness is considered.
The Facts - Key Facts
- Many countries, particularly low-and-middle-income countries (LMICs) face a ‘double burden’ of cancer exposures, the most common of which is cancer-causing infections such as cervical and liver cancers are associated with infections with HPV and HBV, respectively.
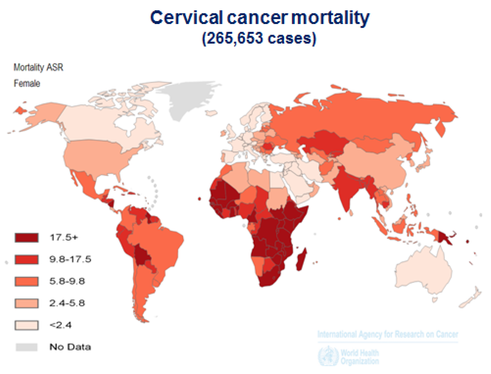
- The global burden of cervical cancer is high and inequitable. An estimated 528,000 women get cervical cancer each year, and 266,000 die. 85% of these women are in developing countries. The global cost of cervical cancer was $2.7 billion per year in 2010. This will rise to $4.7 billion by 2030.
- The currently available HPV vaccines can prevent approximately 70% of cervical cancer cases. These two vaccines have been shown to be at least 90% effective in preventing persistent HPV 16 and 18 infections – the cause of most cervical cancers. As of the end of 2011, 40 countries had introduced HPV vaccines in their national immunisation schedule.
- In 2012, there were 745,000 deaths from liver cancer with 83% (50% in China alone) of cases occurring in developing countries, with chronic infection with Hepatitis B Virus (HBV) a major cause, accounting for approximately 50-55% of cases. HBV infection acquired in infancy and childhood increases the risk of developing cancer later in life.
Liver Cancer – Both Sexes – 2012

Meeting the Challenge
Financial Accessibility: One of the greatest barriers to universal introduction of HPV immunisation programmes is cost. Progress towards affordable pricing for HPV vaccine is being driven by the GAVI Alliance, with GAVI opening a window of support for eligible countries for the introduction of the HPV vaccine at either the national level or as a demonstration project, greatly increasing the capacity of low-income countries to deliver this vaccine.
Cervical Cancer Prevention Continuum: The HPV vaccine is best introduced as part of a comprehensive strategy to prevent cervical cancer. Pre-cancerous lesions of the cervix caused by persistent HPV infection are detectable prior to progression to invasive cancer, and are treatable.
Routine screening and treatment has dramatically reduced cervical cancer morbidity and mortality in wealthier nations and innovative “screen and treat” approaches for lower income settings have been shown to be effective. Coupling the vaccination of girls with screening and treatment of women will be the most effective strategy to rapidly reduce the cervical cancer burden.

A girl receives the HPV vaccine in Laos, South East Asia. Photo: WHO/Bart Verweij.
Universal Coverage of HBV Vaccine: Today, most countries provide pentavalent vaccine, a 5-in-1 shot vaccine that combines protection against hepatitis B with diphtheria, tetanus, pertussis and Haemophilus influenzae type b (Hib). HBV should be included in immunisation schedules, in particular the first dose at birth in national plans.
Key Tools
Country Example
China’s dramatic fall in Hepatitis B infections: Just over a decade ago, barely 40% of children in China’s poorest areas were immunised against hepatitis B (hepB). Approximately 10% of China’s population were chronic carriers of the disease, which is responsible for hundreds of thousands of deaths every year in China due to liver cancer and cirrhosis.
In 2002, GAVI, the Government of China and the China Centre for Disease Control (CDC) started a partnership that lasted until December 2010 to combat the disease. The collaboration provided first-dose hepB vaccines at birth free of charge to over 25 million newborns in the poorest and most remote provinces of western and central China.
But health authorities faced formidable challenges. Immunising babies at birth was difficult as women in remote areas mostly gave birth at home. Raising public awareness of the value of immunisation and encouraging mothers to deliver in hospitals was therefore important. Chinese Government decided to introduce the vaccine into its routine immunisation programme in 2005. Since the start of the project, the percentage of newborn children immunised with the first dose at birth has climbed from 64% to over 90% in most areas. Less than 1% of children under 5 are now chronic carriers of hepB.
